Sexual Health Quarters offers an accessible and inclusive service. Anyone with a cervix is welcome to make a cervical screening appointment with our experienced clinicians. We can offer supported appointments for individuals who may need extra assistance.
As of July 2022, people with a cervix have greater choice in screening options for the Cervical Screening Test (CST). This means that if you have a cervix, are 25-74 years of age and have ever been sexually active, you will have two options for your cervical screening:
- Your clinician collecting the sample for you
- You collect the sample on your own (more information below)
The cervix is where the vagina meets the uterus, it has a small hole that opens to the uterus. If someone is pregnant, the cervix helps to keep bacteria out of the womb. When a birth occurs, the baby passes through the cervix.
Cervical screening changed in Australia in late 2017. The Pap smear was replaced with a new, more accurate Cervical Screening Test. The new test looks for the cause of most cervical cancer, human papilloma virus (HPV). If you’ve had a Pap smear before, the way the test is done will look and feel the same. The procedure might be a bit uncomfortable, but it shouldn’t be painful.
If you are a person with a cervix aged 25-74 years, and have ever been sexually active, you should have a Cervical Screening Test every five years until the age of 74. Your first test is due at 25 years of age.
This includes those who:
- Feel well and have no symptoms
- Are pregnant
- Have been vaccinated against HPV
- Are going through menopause
- No longer have periods
- Have not had sexual contact in a long time
- Have only ever had one sexual partner
- Have an intellectual and/or physical disability
- Only have sex with women
- Are transgender, gender diverse or non-binary and have a cervix
Regular screening can help keep your cervix healthy.
The purpose of CSTs is to look for the Human Papilloma Virus (HPV). HPV can cause cell changes on the cervix, which may lead to cancer in the future. These tests are done every five years, starting when you’re 25, and ending once you’re 74.
Over 99% of cervical cancer is caused by HPV. It’s a common sexually transmissible infection (STI) with up to 90% of people having at least one genital type of HPV at some point in their life. Most HPV infections go away on their own and don’t cause problems. There are many different strains of HPV, but some of them (like strains 16 and 18) can cause cervical cancer.
Some ways to reduce the risk of getting HPV include having the HPV vaccine and using condoms and dams during sex. However, because HPV is transmitted through genital skin contact (and not just sex) they don’t provide 100% protection against HPV.
This means that testing is the best way to prevent cervical cancer caused by HPV.
The HPV vaccine does not protect against all types of HPV that can cause cervical cancer, so it is important to continue regular screening even after having the HPV vaccine.
Collecting your own sample and having your healthcare provider collect your sample are both accurate, safe, and effective ways to screen for cervical cancer. Some people may prefer the privacy and ease of collecting the sample themselves – you get to decide if this is what you’d like to do.
What’s the difference between clinician collected CST and self-collected?
Clinician collected sample
A speculum is used to gently open the vagina so the cervix can be seen well, and a sample of cells from the cervix is taken using a small brush which tests for HPV. While the sample is taken, the clinician will also check for any other issues that might require follow up. If the sample shows that HPV is present, the laboratory will use the same sample to test for any cervical cell changes.
Cervical screening may feel uncomfortable, but it shouldn’t be painful. You are allowed to tell the clinician if you are in pain, as you have control of the situation. Some people may find a cervical screen embarrassing or feel uncomfortable with the idea. Don’t be afraid to talk to your doctor about this, as there are things they can do to make you more comfortable, or you can try self-collection:
Self-collected sample
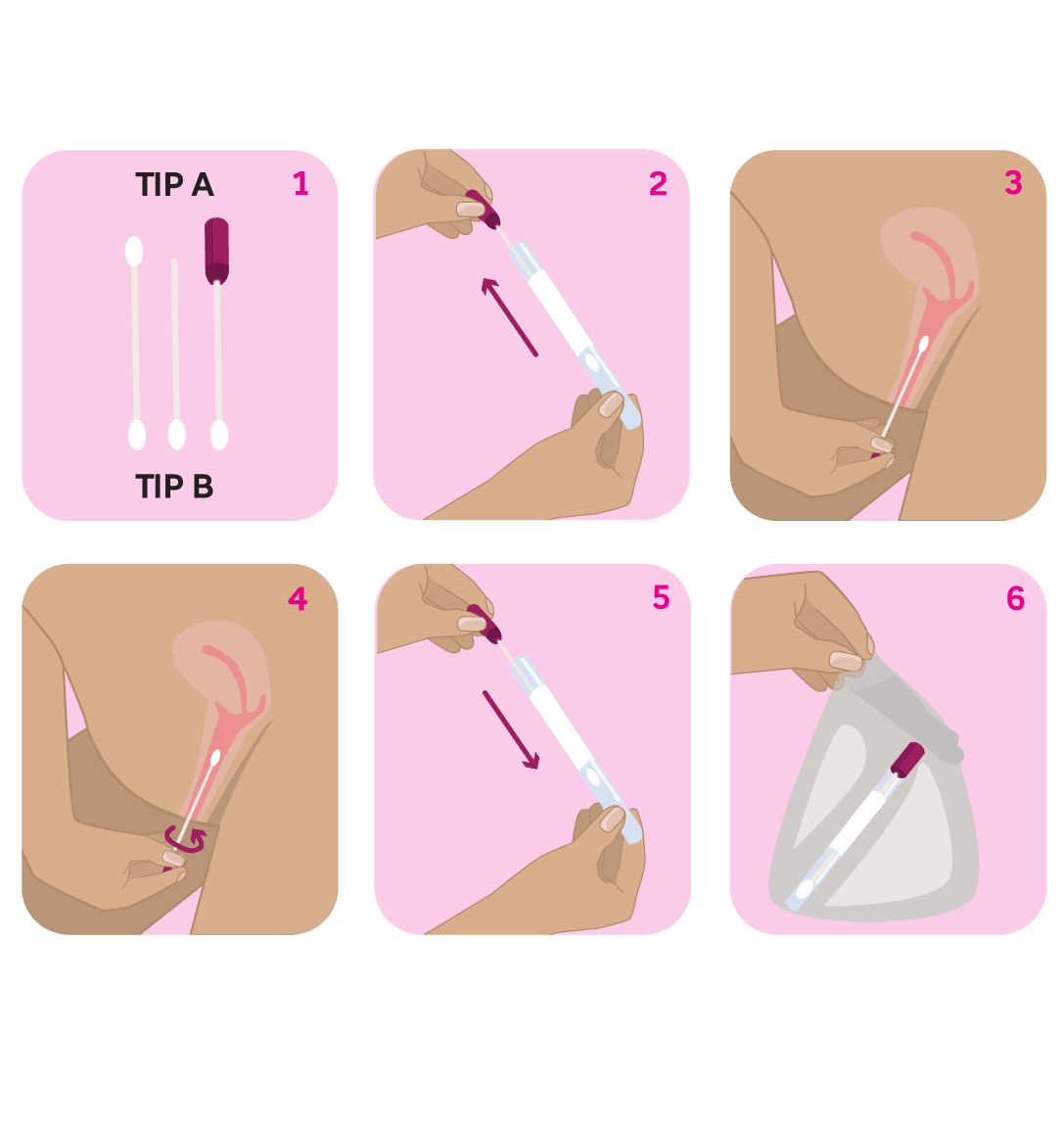
The clinician will give you instructions and a specially designed swab so you can take the sample yourself in a private area at the clinic.
Here is how it is done:
Self-collection tests for HPV only, as the sample does not contain cervical cells required for further testing. If HPV is found, you will need to complete a cervical screening examination with a clinician.
Negative means there was no HPV detected and your next CST should be in five years (unless advised otherwise by the clinician). A negative result indicates you are at low risk of developing cervical cancer.
If you develop symptoms at any time during the five-year period (e.g., abnormal bleeding or abnormal discharge), you should go back to your doctor. Don’t wait for your next CST, even if your last one was only a couple of months ago.
Positive means HPV was detected. This does not mean you have cervical cancer, but the presence of the infection means you may be at greater risk of cervical cancer in the future. If HPV is detected, lab clinicians will also check for abnormal cells.
Cervical screening tests look for “higher risk” types of HPV (types 16 and 18), and for other types that give an “intermediate” risk of later getting cancer of the cervix.
HPV non 16/18 (intermediate risk)
If you have taken your own test and get an “intermediate” result, you will be asked to come back for a clinician to collect a sample. This sample will contain cells from the cervix to be tested for possible changes that could lead to cervical cancer. If there are significant changes, you will be then referred for colposcopy.
If you’ve been asked to come back in 12 months
For people with intermediate risk, (HPV non 16/18 and no minor changes) it is safe to wait. It usually takes several years to go from something minor to significant, so there is plenty of time to check things. Often HPV disappears on its own, so no extra tests would be needed if the result is clear in 12 months’ time.
HPV 16 or 18 (higher risk)
HPV 16 and 18 are the higher risk strains. They can often disappear on their own, or they can persist but not cause cancer. Sometimes they will cause cell changes over a long period of time which lead to cancer if it’s not treated. If you have a HPV 16 or 18 result, you will be referred for a colposcopy.
If you’ve been referred for a colposcopy
A colposcopy is when a speculum is inserted, and the cervix is looked at through a microscope. The cervix may be painted with acetic acid or iodine to show the clinician where abnormal cells are. A small sample of tissue (a biopsy) may be taken for testing. A colposcopy should not be painful but can be uncomfortable or feel a little odd. You are allowed to ask for assistance if you’re feeling uncomfortable.
If the tissue tests positive for abnormal cells (called high-grade squamous intraepithelial lesion (HSIL), then this may need to be removed in a surgical procedure. You will then need two consecutive yearly negative CST results before you can go back to five yearly screening.
Download our Cervical Screening Test information sheet
For more information about cervical screening go to http://www.healthywa.wa.gov.au/cervicalscreening
Cervical Screening Program

Paid Volunteers Needed: CST Simulated Patient
Cervical screening simulated patients are used by SHQ three times per year (within business hours) to help train nurses and doctors in cervical screening. Simulated patients will be given a fictional name and simple medical history to use within the training consultation. The cervical screening test taken during the consultation will be disposed of and will not be sent to pathology for testing.
Payment for your time is $50 per examination. Please fill out the expression of interest form below if you would like to participate.
Cervical Screening Test Simulated Patient Expression of Interest Form
Cervical screening simulated patients are used by SHQ three times per year (within business hours) to help train nurses and doctors in cervical screening. Simulated patients will be given a fictional name and simple medical history to use within the training consultation. The cervical screening test taken during the consultation will be disposed of and will not be sent to pathology for testing.
Please note: this is not a cervical screening booking form. To book a cervical screening test at SHQ, call us on 08 9227 6177 or click the link below.
"*" indicates required fields