Download PDF Information Sheet
This information is designed to be used in consultation with your health professional. Read our Legal Disclaimer here.
A guide to self-collected cervical screening, HPV, and your test results
Since July 2022 the National Cancer Screening Program will be providing greater choice in screening options for the Cervical Screening Test (CST). This means that if you have a cervix, are 25-74 years of age and have ever been sexually active, you will have two options for your cervical screening:
- Your clinician collecting the sample for you
- You collect the sample on your own
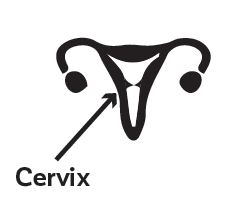
The cervix is where the vagina meets the uterus. It has a small hole that opens to the uterus. If someone is pregnant, the cervix helps to keep bacteria out of the womb. When a birth occurs, the baby passes through the cervix.
Regular screening can help keep your cervix healthy. The purpose of CSTs is to look for the Human Papilloma Virus (HPV). HPV can cause cell changes on the cervix, which may lead to cancer in the future. These tests are done every five years, starting when you’re 25, and ending once you’re 74.
Over 99% of cervical cancer is caused by HPV. It’s a common sexually transmissible infection (STI) with up to 90% of people experiencing at least one genital type of HPV in their life.
Most HPV infections go away on their own and don’t cause problems. There are many different strains of HPV, but some of them (like strains 16 and 18) can cause cervical cancer.
Some ways to reduce the risk of getting HPV include having the HPV vaccine and using condoms and dams during sex. However, because HPV is transmitted through genital skin contact (and not just sex) they don’t provide 100% protection against HPV.
This means that testing is the best way to prevent cervical cancer caused by HPV.
Clinician collected
A speculum is used to gently open the vagina so the cervix can be seen well, and a sample of cells from the cervix is taken using a small brush which tests for HPV. While the sample is taken, the clinician will also check for any other issues that might require follow up. If the sample shows that HPV is present, the laboratory will use the same sample to test for any cervical cell changes.
Cervical screening may feel uncomfortable, but it shouldn’t be painful. You are allowed to tell the clinician if you are in pain, as you have control of the situation. Some people may be uncomfortable with a clinician collecting the sample for a variety of reasons and that’s ok.
Self-collected sample
The clinician will give you instructions and a specially designed swab so you can take the sample yourself in a private area at the clinic. Here is how it is done:
2. Before starting
Your healthcare provider will give you a package. Inside is a swab. Your swab may look different to those pictured here. Before you open the package, make sure you know which end of the swab can be held (Tip A), and which end is for taking the sample (Tip B). If you are unsure which end is which, ask your healthcare provider for advice. Before taking the sample make sure your hands are clean and dry. Make sure you are in a comfortable position and your underwear is lowered.

2. Preparing the swab
Twist the cap and remove the swab from the packaging. Make sure not to touch Tip B that will be inserted to collect the sample. Do not put the swab down.

3. Inserting the swab
Use your free hand to move skin folds at the entrance of your vagina. Gently insert Tip B into your vagina (similar to inserting a tampon). The swab may have a line or mark on it showing how far to insert.

4. Taking the sample
Rotate the swab gently for 10-30 seconds; this should not hurt, but may feel a bit uncomfortable.

5. Storing the sample
Still holding on Tip A, gently remove the swab from your vagina. Place the swab back into the packaging with Tip B going in first. Screw the cap back on and return the package to your healthcare provider.

6. Sending the sample
The sample will be sent to a pathology laboratory for HPV testing. The results of the test will be sent to your healthcare provider.

Some people may prefer the privacy and ease of collecting the sample themselves. You get to decide if this is what you’d like to do.
- This sample will only include vaginal cells (not cells from your cervix) and can only be tested for HPV. If HPV is detected, you may have to come back for a clinician collected test.
- Without a clinician doing an examination, vulval, vaginal or cervical abnormalities may be missed.
- It isn’t suitable if you’re following up abnormal results, or if you have symptoms e.g., abnormal bleeding or discharge.
- If you’ve had a bad experience with a CST, or are uncomfortable (for any reason), you may prefer to do self-collection. You are allowed to choose what you feel most comfortable doing.
- Self-collected vaginal samples are as safe and accurate as tests taken by a clinician.
Negative means there was no HPV detected and your next CST should be in five years (unless advised otherwise by the clinician). A negative result indicates you are at low risk of developing cervical cancer.
If you develop symptoms at any time during the five-year period (e.g., abnormal bleeding or abnormal discharge), you should go back to your doctor. Don’t wait for your next CST, even if your last one was only a couple of months ago.
Positive means HPV was detected. This does not mean you have cervical cancer, but the presence of the infection means you may be at greater risk of cervical cancer in the future. If HPV is detected, lab clinicians will also check for abnormal cells.
Cervical screening tests look for “higher risk” types of HPV (types 16 and 18), and for other types that give an “intermediate” risk of later getting cancer of the cervix.
HPV non 16/18 (intermediate risk)
If you have taken your own test and get an “intermediate” result, you will be asked to come back for a clinician to collect a sample. This sample will contain cells from the cervix to be tested for possible changes that could lead to cervical cancer. If there are significant changes, you will be then referred for colposcopy.
If you’ve been asked to come back in 12 months
For people with intermediate risk, (HPV non 16/18 and no minor changes) it is safe to wait. It usually takes several years to go from something minor to significant, so there is plenty of time to check things. Often HPV disappears on its own, so no extra tests would be needed if the result is clear in 12 months’ time.
HPV 16 or 18 (higher risk)
HPV 16 and 18 are the higher risk strains. They can often disappear on their own, or they can persist but not cause cancer. Sometimes they will cause cell changes over a long period of time which lead to cancer if it’s not treated. If you have a HPV 16 or 18 result, you will be referred for a colposcopy.
If you’ve been referred for a colposcopy
A colposcopy is when a speculum is inserted, and the cervix is looked at through a microscope. The cervix may be painted with acetic acid or iodine to show the clinician where abnormal cells are. A small sample of tissue (a biopsy) may be taken for testing. A colposcopy should not be painful but can be uncomfortable or feel a little odd. You are allowed to ask for assistance if you’re feeling uncomfortable.
If the tissue tests positive for abnormal cells (called high-grade squamous intraepithelial lesion (HSIL), then this may need to be removed in a surgical procedure. You will then need two consecutive yearly negative CST results before you can go back to five yearly screening.
With the combination of the HPV vaccination in all teenagers, and regular screening for people with a cervix, cervical cancer could be eradicated by 2030!
Yes! It’s safe because:
- Cervical cancer is very rare in young people
- The HPV vaccination offers some protection for young people
- HPV is common in young sexually active people and usually clears up by itself
- The cervical screening program has not made a difference to the detection of cervical cancers for people under 25
Yes! It’s still important to have your regular CST. The vaccine prevents most types of HPV infection, but it does not prevent all types that can cause cervical cancer. Talk to a health clinician if you missed out on the HPV vaccine at school, as it may still be useful for you to have it.
It’s your choice whether you discuss your CST results with your partner. It’s likely your partner has HPV too, as it’s very common. There is no way of knowing if your partner currently has it or has had it previously. If your partner/s have a cervix, you can ask if they are up to date with CSTs. Remember, most of the time your body clears the virus without causing any problems.
The National Cervical Screening Register will send you a letter inviting you to have a CST when you turn age 25. Then if your test is negative, your next test will be in 5 years’ time.
Information last updated June 2024
Print copies of select resources can be purchased by visiting our Opens in a new window:Online Shop or Ordering Resources page.